Before the contact lenses were popularized in the 1950s, people suffering from vision problems have been relying on eyeglasses for more than seven centuries. Although it is the earliest and most practical means to correct refractive vision errors, people have eventually got tired of the heavy frames and large lenses of these glasses.
With medical advancements, more advanced procedures are offered nowadays. These procedures range from surgical insertion of artificial lenses to the ablation of the cornea through the use of laser technology. Such methods aim to provide permanent solution and eradicate the reliance on artificial lenses.
The Evolution
For more than two decades, the surgical tools, techniques and procedures used in corrective eye surgeries have rapidly evolved. The tools and techniques have been refined to achieve a more precise result. Eventually, newer procedures were developed in an attempt to compensate the limitations of a previous system.
Radial Keratotomy
The precursor of all corrective eye surgeries, Radial Keratotomy (RK) was widely used in the United States during the 1980s. The surgeons cut spoke-like incisions on the patient’s cornea primarily to correct conditions of nearsightedness.
Unfortunately, long-term results were unfavorable for some individuals. It created problems like significant glare, fluctuating vision, regression and night vision problems for many patients.
Later on, the procedure underwent various modifications and enhancements to minimize its side-effects. This paved the way to laser vision correction procedures. At present, RK is no longer widely practiced by eye surgeons.
LASIK and Other Refractive Eye Surgery Procedures
Photorefractive Keratectomy
Photorefractive Keratectomy (PRK) was the first successful procedure that used laser technology to remove tissues from the eye’s surface and reshape the cornea. It received FDA approval in 1995 and is still commonly used today.
In this process, a thin layer of the cornea’s outer layer is completely removed to expose the area that requires ablation. Using an excimer laser, the excess tissues in the cornea are removed until its desired curvature is achieved. Since no flap is created in PRK, new epithelial cells are developed to cover the eye’s surface.
Pros:
PRK is ideal for patients whose cornea is too thin to undergo LASIK or those who have undergone LASIK before with thinner residual cornea. This is a better option for people with chronically dry eyes, too. There are also no risks of flap complications, like epithelial inagrowth.
Since it does not create corneal flap, the entire underlying stroma is available during treatment. Hence, it does not compromise the corneal thickness and the laser does not reach deeper tissues.
Cons:
PRK has comparatively slower recovery rate. This is because the epithelial cell takes longer time to grow back. It takes longer to achieve the best vision, too. In the early stage of recovery, PRK patients experience more discomfort than those who underwent LASIK. Finally, there are higher risks of post-surgery infection, haze and inflammation.
Laser-Assisted in situ Keratomileusis
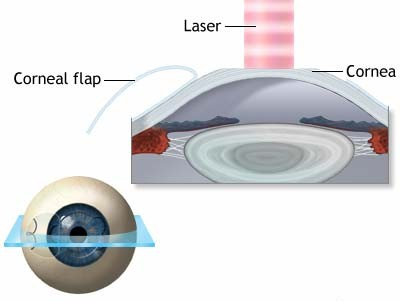
The result of PRK can be comparable to that of LASIK surgery. This is because the two procedures are closely similar except that LASIK creates a flap from the epithelial layer to reach the underlying tissues. After the operation, the flap is repositioned to serve as natural bandage.
Pros:
LASIK has shorter recuperation period because regeneration of epithelial cells is much faster than the growth of new cells. The postoperative discomfort is usually mild and short-term. In fact, many patients can see normally a few hours after their operation. Their vision gradually improves before reaching peak quality after several weeks.
Cons:
The removal of thin flap from the cornea’s outer layer makes LASIK not suitable for patients with thin cornea. It also has the tendency to aggravate dry eye conditions. There have been reported cases of errors in the repositioning of the epithelial flap.
Laser Epithelial Keratomileusis
A variant of PRK, the Laser Epithelial Keratomileusis (LASEK) also removes the outer layers of the cornea completely. It uses an alcohol solution to loosen the epithelial cells before lifting it. LASEK uses laser technology, too, in reshaping the cornea.
After the operation, the flap is replaced. The patient will have to wear soft contact lenses in the first few days following the surgery to secure the flap in place while it heals.
Pros:
LASEK is a less aggressive form of PRK. It is an ideal option for people with thin corneas who cannot undergo LASIK. This is also more effective for patients with higher prescription. Since only the outer surface layers are removed, the surgeon has more corneal tissues to work with.
Cons:
LASEK takes longer time to recover full vision compared to LASIK. After the operation, the patient also feels more uncomfortable.
Bladeless/All-Laser LASIK
Instead of using mechanical cutting tool, using laser in creating the flap out of the epithelial layer is another option. This is sometimes referred to as IntraLASIK because the laser used for this purpose was originally developed by IntraLase Corp. The use of laser and computer-aided technology grants the surgeon better control over the size and thickness of the flap to be created.
Once the outer layer was removed, another type of laser, the excimer, is used to change the shape of the cornea’s curvature.
Pros:
Considered a superior form of LASIK, this procedure offers a more accurate result with fewer risks. Possible long-term damage on the cornea with traditional LASIK is also underplayed because of precision. Vision can be restored in a matter of hours, so the patient may return to work in a couple of days.
Cons:
The sole disadvantage of this procedure is its cost. This is one of the most expensive refractive eye surgeries at present.
Which Procedure is Right for You?
Without a doubt, these refractive eye surgeries are all safe and effective. These also carry high patient satisfaction rate. Thanks to the continuous progressions in medical technology, major drawbacks of every operation are being improved.
All the same, certain conditions make a candidate more suitable for a certain procedure than the others. The best person to ask for recommendations will be a trained eye doctor. You will be subjected to preoperative consultations and examinations to identify which surgery works best for you. The great news is that no matter what procedure you choose, you will most certainly be pleased with its results.